
SSI-Related Medicaid Fact Sheet 1
SSI-RELATED MEDICAID
FACT SHEET
This Fact Sheet provides a general description and a brief overview of information about the
coverage groups for individuals who are aged, blind, or disabled. The Department of Children
and Families (DCF) determines eligibility. Federal regulations, Florida Statutes, and Florida
Administrative Rule contain specific policies for eligibility.
Note: The income standards generally change effective January and April of each year.
June 2022
SSI-Related Medicaid Fact Sheet 2
Table of Contents
Contact Information ............................................................................................................. 3
Overview of Program .......................................................................................................... 4
Eligibility Requirements ....................................................................................................... 5
Coverage Groups with Full Benefits .................................................................................... 6
Medicaid for Aged and Disabled (MEDS-AD) ..................................................................... 6
Institutional Care Program (ICP) ......................................................................................... 6
Hospice ............................................................................................................................... 6
Program of All-Inclusive Care for the Elderly (PACE) ......................................................... 6
Modified Project AIDS Care (MPAC) .................................................................................. 7
Home and Community Based Services (HCBS) Waivers ................................................... 7
Familial Dysautonomia (FD) Waiver ................................................................................... 7
iBudget Waiver ................................................................................................................... 7
Model Waiver ...................................................................................................................... 8
Statewide Medicaid Managed Care, Long – Term Care (SMMC LTC) Waiver ................... 8
Additional Information for ICP, Hospice, HCBS and PACE Coverage Groups .................... 9
Qualified Income Trust (QIT) .............................................................................................. 9
Uncovered Medical Expense Deduction (UMED) ............................................................. 11
Special Policies that Apply to Spouses ............................................................................. 11
Calculating Patient Responsibility (PR) ............................................................................ 12
Long Term Care (LTC) Insurance Partnership Program .................................................... 13
Coverage Groups with Limited Benefits ........................................................................... 15
Medically Needy ............................................................................................................... 15
Qualified Medicare Beneficiaries (QMB) ........................................................................... 15
Specified Low-Income Medicare Beneficiaries (SLMB) .................................................... 15
Qualifying Individuals 1 (QI-1) ........................................................................................... 15
Breast and Cervical Cancer Treatment (BCC) .................................................................. 15
Optional State Supplementation (OSS) ............................................................................ 16
Home Care for the Disabled Adult (HCDA) ....................................................................... 16
Extra Help with Medicare Prescription Drug Plan Costs ................................................... 16
Additional Resources for Assistance ................................................................................ 17
My ACCESS Account – Provider View Guide ................................................................... 19
Where to Find Customer’s Patient Responsibility Amount in Provider View ..................... 20
SSI-Related Medicaid Fact Sheet 3
CONTACT INFORMATION
Department of Children and Families (DCF)
The Department of Children and Families main website is at: http://www.myflfamilies.com/
Individuals may apply for Medicaid:
•
On-line at the DCF/Automated Community Connection to Economic Self
Sufficiency (ACCESS) Florida website at: https://www.myflorida.com/accessflorida/
•
On-site at a DCF/ESS Customer Service Center. To locate a service center,
“Select a County” from the “Find Your Service Center” option at:
https://www.myflfamilies.com/service-programs/access/map.shtml
•
On-site through a member of the DCF Community Partner Network. Community
partners are listed at: https://access-web.dcf.state.fl.us/CPSLookup/search.aspx
•
By submitting a paper application or completing a telephonic application which
may be done by calling 1-850-300-4323, submitting it in person, by mail or fax.
Customer Service Center locations and fax numbers can be found at:
https://www.myflfamilies.com/service-programs/access/map.shtml
Individuals may check their case status using their My ACCESS Account on the
ACCESS Florida website at: http://www.myflorida.com/accessflorida/. The website is
available 24 hours a day, 7 days a week. After registering, you can:
•
Check on the status of an application or renewal
•
View when the next renewal is scheduled
•
Complete an annual renewal
•
View a list of items needed to process the application or renewal
•
View the date and time of a scheduled appointment
•
View the Share of Cost amount if enrolled in Medically Needy
•
View the amount of the patient responsibility
•
Print a temporary Medicaid card
•
Upload and view documents
•
Report household changes
Information may also be accessed by calling the Interactive Voice Response (IVR)
Phone System, which is an automated response system available by phone at 1-850-
300-4323. Also available is the DCF’s Virtual Assistant chat assistant on the website at:
http://www.myflorida.com/accessflorida/.
Community Partner Agencies
Community Partner Agencies work with the ACCESS Florida Program by providing a variety
of services to individuals seeking or receiving Food, Cash, or Medical assistance. To find a
local Community Partner Agency in your area, go to:
https://access-web.dcf.state.fl.us/CPSLookup/search.aspx
SSI-Related Medicaid Fact Sheet 4
OVERVIEW OF PROGRAMS
Medical Assistance:
Medicaid is a federal and state program that is administered by the Agency for Health Care
Administration (AHCA). States are allowed options in the administration of their Medicaid
program. The eligibility requirements and available services may vary from state to state.
Medicaid eligibility is determined by DCF, except for recipients of Supplemental Security
Income (SSI). Individuals who receive SSI are automatically entitled to Medicaid in Florida.
Medicaid services are managed by AHCA. DCF determines eligibility for the following SSI-
Related Medicaid Coverage Groups:
•
Medicaid coverage groups that have full benefits include:
o
Medicaid for aged and disabled individuals (MEDS-AD)
o
Modified Project Aids Care (MPAC)
o
Institutional Care Program (ICP)
o
Hospice
o
Home and Community Based Services (HCBS) Waiver
o
Program of All-Inclusive Care for the Elderly (PACE)
•
Medicaid coverage groups that have limited benefits include:
o
Medically Needy (MN)
o
Medicare Savings Programs (MSP):
Qualified Medicare Beneficiary (QMB)
Specified Low-income Medicare Beneficiary (SLMB)
Qualifying Individuals 1 (QI-1)
Working Disabled (WD)
Low Income Subsidy (LIS)
Automatic Entitlement to Medicaid Coverage
An individual receiving cash benefits from the Social Security Administration’s (SSA), SSI
Program is automatically eligible for Medicaid. A separate application is not required when
Medicaid coverage is through SSI. When the cash benefits terminate, the individual may
be entitled to additional months of Medicaid coverage. If the SSI terminates, Medicaid
coverage will continue for two months beyond the SSI payment end date to allow time for
DCF to review eligibility under other coverage groups.

SSI-Related Medicaid Fact Sheet 5
SSI-RELATED MEDICAID ELIGIBILITY REQUIREMENTS
Eligibility for individuals who are either aged (65 or older) or disabled is referred to as
SSI- Related Medicaid. The information below provides basic eligibility criteria. Some
coverage groups require additional technical criteria specifically for that coverage.
•
Aged, Blind or Disabled – an individual must be aged (65 or older) or, if under age
65, blind or disabled. Note: The disability must prevent the individual from working
and be expected to last for a period no less than 12 months or be expected to result
in death. Individuals who receive a disability check from the Social Security
Administration (SSA) based on their own disability automatically meet this
requirement. A disability determination is completed by SSA or the state Division of
Disability Determinations (DDD). DCF submits requests to DDD after the Medicaid
application is received.
•
Citizenship Status – an individual must be a U.S. citizen or a qualified non-citizen.
Note: There may be a waiting period for non-citizens admitted to the U.S. with a
qualified status on or after August 22, 1996.
•
Identity – an individual must provide proof of identity. Exceptions: individuals
receiving SSI, Medicare or Social Security Disability based on their own work history.
•
Florida Resident - residency exists when the intent of the individual is to remain in
the state. Residency does not exist when the stay is for a temporary purpose such
as a vacation and there is intent to return to a residence in another state.
•
Social Security Number – an individual must have a social security number or apply
for one.
•
File for Other Benefits – an individual must apply for other benefits for which they
may be eligible (i.e. - pensions, retirement, disability benefits, etc.).
•
Report Third Party Liability – examples include health insurance or payments by
another party.
•
Income – each coverage group has a specific income limit, see link below.
•
Resources – each coverage group has a specific resource limit, see link below.
Note: Additional information and criteria are provided in this document by coverage
group.
The SSI-Related Medicaid Financial Eligibility Standards chart is located at:
https://www.myflfamilies.com/service-programs/access/docs/esspolicymanual/a_09.pdf

SSI-Related Medicaid Fact Sheet 6
COVERAGE GROUPS WITH FULL BENEFITS
Medicaid for Aged and Disabled (MEDS-AD)
•
Medicaid for low-income individuals who are either aged (65 or older) or disabled.
•
This coverage group does not include blind individuals unless they are disabled.
Institutional Care Program (ICP)
•
The Institutional Care Program (ICP) helps individuals in nursing facilities pay for
the cost of their care and other medical services.
•
Additional technical criteria include:
o
An evaluation to need nursing facility services and appropriate placement
as determined by the Department of Elder Affairs (DOEA),
Comprehensive Assessment and Review for Long-Term Care Services
(CARES) process to determine the level of care (LOC).
o
Other important criteria for ICP eligibility include:
Transfer of Assets – assets transferred on or after January 1, 2010,
may potentially affect eligibility. The “look-back” period for asset
transfers is 60 months prior to the application month.
Spousal Allowance – assets and income are evaluated for married
individuals when one spouse is institutionalized, and one spouse
continues to reside in the community (referred to as the “community
spouse”). The community spouse (CS) may be eligible to receive a
portion of the institutionalized spouse’s income.
•
Additional information on forms and instructions is located on AHCA’s website for
Medicaid Nursing Facility Provider Information.
Hospice
•
Hospice services help maintain care for terminally ill individuals. T o
receive Hospice care, the individual must enroll in Hospice.
•
Additional technical criteria include:
o
A medical prognosis that life expectancy is six months or less,
o
Election of hospice services, and
o
A certification of the individual’s terminal illness by a physician or medical
director.
Program of All-Inclusive Care for the Elderly (PACE)
• PACE provides home and community-based services for individuals in need of
nursing facility care as assessed by DOEA CARES. Once enrolled in PACE, an
individual may continue services even if the individual is admitted to an assisted
living facility (ALF) or nursing home. More information can be found at:
http://www.ahca.myflorida.com/
•
Additional technical criteria include:
o
election of a PACE provider as the sole source of Medicare and/or
Medicaid service delivery,
o
at least age 55 or older (must meet disability criteria if under age 65), and
o
meet a nursing home LOC as determined by CARES.
Note: PACE is not a waiver but individuals who are potentially eligible under this coverage
group may apply directly with DCF. When applying, the applicant should select “Medical
Assistance for Individuals Seeking Medicaid Waiver Services
”.

SSI-Related Medicaid Fact Sheet 7
Modified Project AIDS Care (MPAC)
•
MPAC is a Managed Medical Assistance Program for individuals with Acquired
Immune Deficiency Syndrome (AIDS) who are not eligible for any other full
Medicaid coverage group
.
• Additional technical criteria include:
o be at or below 300 percent of the Federal Benefit Rate (FBR),
o at least 18 or older (must meet disability criteria if under age 65), and
o meet presumptive disability criteria as evidenced by AHCA Form 5000-0607,
Acquired Immune Deficiency Syndrome (AIDS), Physician Referral for
Individuals at Risk of Hospitalization
Note: MPAC is not a waiver but individuals who are potentially eligible under this coverage
group may apply directly with DCF. When applying, the applicant should select “Medical
Assistance for Individuals Seeking Medicaid Waiver Services”.
Home and Community Based Services (HCBS) Waivers/ Working People with
Disabilities
•
HCBS Waivers allow individuals at risk of institutionalization to receive the essential
services necessary to maintain an independent lifestyle while residing in the
community
.
• HCBS Waivers are:
o Familial Dysautonomia (FD) Waiver
o iBudget Waiver
o Model Waiver
o Statewide Medicaid Managed Care Long – Term Care (SMMC LTC) Waiver
• The Working People with Disabilities (WPwD) eligibility criteria allow a higher
income, and asset thresholds, when necessary, for individuals with earned income
and enrolled in an HCBS waiver.
Familial Dysautonomia (FD)
•
For individuals diagnosed with FD syndrome who would otherwise require
hospitalization if not receiving special services.
•
Contact AHCA to initiate the waiver request. More information is available at:
https://ahca.myflorida.com/Medicaid/hcbs_waivers/fd.shtml
•
Additional technical criteria include:
o
enrollment in the FD Waiver,
o
age three or older (must meet disability criteria if under age 65), and
o
meet LOC for being at risk of hospitalization as determined by CARES.
iBudget
•
For individuals with a developmental disability to live in the community as
assessed by the Agency for Persons with Disabilities (APD). More information
is available at: http://www.apd.myflorida.com/.
• Additional technical criteria include:
o enrollment in the iBudget,
o age three or older (must meet disability criteria if under age 65), and
o
meet LOC determination by APD
.
SSI-Related Medicaid Fact Sheet 8
Model Waiver
•
Formerly known as the Katie Beckett Waiver, provides services to individuals
with degenerative spinocerebellar disease
.
•
Contact AHCA to initiate the waiver request. More information is available at
:
https://ahca.myflorida.com/Medicaid/hcbs_waivers/model.shtml.
•
Additional technical criteria include:
o
enrollment in the Model,
o
a medical diagnosis of degenerative spinocerebellar disease,
o
under age 21 and disabled, and
o
meet a LOC for inpatient hospital care as determined by the Children’s
Medical
Services (CMS).
Statewide Medicaid Managed Care, Long-Term Care (SMMC LTC) Waiver
•
SMMC LTC provides services to help prevent institutionalization by allowing an
individual to live in the community as assessed by DOEA CARES
.
More
information can be found at: https://ahca.myflorida.com/Medicaid/statewide_mc/.
•
Additional technical criteria include:
o
enrollment in the SMMC LTC Waiver,
o
be 18 years of age or older (must meet disability criteria if under 65), and
o
meet a nursing home LOC as determined by CARES.
•
Contact their local Aging and Disability Resource Center (ADRC) to be screened for
services.
Provides services for adults with Cystic Fibrosis (CF),
Traumatic Brain and
Spinal Cord Injury (TBI) and HIV/AIDS
.
DOEA is the contact for SMMC LTC Waiver
for adults. Individuals, their caregivers, and community providers should contact
DOEA for more information:
o
Email: Medwaiver@elderaffairs.org ; Phone: (866) 232-3733 or Fax: (850)
414-2310
o
To find your local ADRC, call the Elder Helpline at 1-800-96-ELDER
(800-963-5337) or go to the Department of Elder Affairs website at:
http://elderaffairs.state.fl.us/doea/arc.php
ADDITIONAL INFORMATION FOR
ICP, HOSPICE, HCBS AND PACE COVERAGE GROUPS
ICP, Hospice, HCBS, PACE, and Modified Project Aids Care (MPAC) coverage groups have
additional income and resource (asset) criteria, which are evaluated during the eligibility
determination process. The additional criteria are discussed on the next few pages
.
Qualified Income Trust (QIT) What is a Qualified Income Trust?
If an individual’s income is over the limit to qualify for Medicaid long-term care eligibility (including
nursing home care), a QIT allows an individual to become eligible by depositing income into an
account each month that the individual needs Medicaid. The QIT involves a written agreement,
establishing a special account, and making deposits into the account.

SSI-Related Medicaid Fact Sheet 9
Who needs a Qualified Income Trust?
An individual needs a QIT if their income before any deductions (such as taxes, Medicare or
health insurance premiums) is over the income limit to qualify for eligibility for ICP, Hospice,
HCBS, PACE coverage groups.
How do I set up a Qualified Income Trust agreement?
Professional help may be obtained to set up the QIT agreement but is not required. A QIT
agreement must meet specific requirements and be approved by the Department of Children
and Families Regional Legal Counsel. A copy of the QIT agreement must be submitted to an
eligibility specialist who will forward these documents for review.
What items must be included in the Qualified Income Trust agreement?
The QIT agreement must:
• Be irrevocable (cannot be canceled).
• Require that the State receive all funds remaining in the trust at the time of
the individual’s death (up to the amount of Medicaid benefits paid).
• Consist of the applicant’s income only (do not include or add assets).
• Be signed and dated by the applicant, the applicant’s spouse, or a person
who has legal authority to act on the applicant’s behalf.
How does the Qualified Income Trust account work?
After setting up the account, the individual must make deposits into the QIT account every
month for as long as Medicaid is needed. This means deposits may be needed before a
Medicaid application is approved. When income is deposited into the QIT account in the
month it is received, it will not be counted in an eligibility determination. Deposits cannot be
made for a past or future month. If a deposit is not made in any given month, or enough
income is not deposited, the individual will be ineligible for Medicaid.
Note: The income placed into a Qualified Income Trust is excluded as income in
the eligibility determination but counted in the calculation of the patient
responsibility
.
How much income must I deposit into the Qualified Income Trust account?
Enough income must be deposited into the QIT account each month so that remaining
income is within coverage group limit(s). It is better to deposit more income than take the
chance of depositing too little to qualify for Medicaid. For information about current income
limits call (850) 300-4323 or visit:
https://www.myflfamilies.com/service-programs/access/docs/esspolicymanual/a_09.pdf

SSI-Related Medicaid Fact Sheet 10
What happens to the income deposited in the Qualified Income Trust account?
The income deposited and withdrawn is used to calculate an individual’s patient
responsibility. If an individual has a patient responsibility, they are responsible for paying
that amount. If funds are left in the QIT upon death, it is paid to the State, up to an amount
equal to the total Medicaid benefits the State paid on behalf of the individual.
How to pay funds remaining in the QIT to the State?
The QIT trustee or other individual acting on behalf of the individual should contact the
long-term care facility to see if any refund for the month of death is due back to the trust.
The balance of the QIT as of the date of death, plus any refund from the long-term care
facility, must be paid to the State.
Mail a check payable to the “Agency for Health Care Administration” and send to:
Florida Medicaid TPL Recovery Program
PO Box 12188
Tallahassee, FL 32317-2188
Phone: 844-845-8352
Email: flsub[email protected]
The Qualified Income Trust Information Sheet can be found at:
https://www.myflfamilies.com/programs/access/docs/qualified_income_trust_factsheet.pdf
Uncovered Medical Expense Deduction (UMED)
What is an Uncovered Medical Expense Deduction (UMED)?
An uncovered medical expense deduction (UMED) is a credit received for out-of-pocket
medical expenses incurred when the individual is eligible for coverage in LTC. The amount
of the deduction is the total of allowed medical expenses that is converted to a monthly
figure.
The deduction reduces the amount the nursing facility or Medicaid services the provider is
paid each month and enables individuals to keep more money to pay for uncovered medical
expenses.
Who can receive the deductions?
Individuals who receive Medicaid under ICP, Hospice, HCBS Waivers (iBudget and SMMC
LTC only) or PACE that have a patient responsibility (share of the cost for care) to pay
from their income may be entitled to the deduction.
SSI-Related Medicaid Fact Sheet 11
What types of medical expenses can be deducted?
Medical expenses include:
• Health insurance costs (premiums, deductibles, and co-payments).
• The cost of medically necessary medical services or items, such as:
o Dental services,
o Hearing supplies and services,
o Vision services and supplies,
o Therapy services,
o Over-the-counter medications, and
o Certain medical supplies such as adult diapers, vitamins, and nutritional
supplements.
• Nursing facilities care not covered by Medicare, Medicaid or another third party.
o Nursing facility bills incurred no earlier than three months prior to the month
of application (paid or unpaid), not paid by Medicaid or another third party,
and were not incurred during a transfer of assets penalty period.
How we determine the deduction and apply it to monthly income?
• Medical expenses paid during a recent period (no earlier than three months
prior to the month of application or the past six months prior to a renewal) are
used to get an average of the expenses expected to occur over the next six
months.
• The average cost is calculated and deducted from the income when calculating
patient responsibility for the next six months. This is called a projection period.
Near the end of a projection period, actual medical expenses incurred during the
projection period are verified and compared to the projected expenses.
• If the projected amount differs from the actual expenses by more than $120,
the expenses are reconciled by averaging the balance over the next projection
period together with an average of actual expenses.
• For some cases this process is repeated every six months while the individual
receives Medicaid.
What must Medicaid recipients do?
Recipients must notify the Department of Children and Families of what medical expenses
(paid or unpaid) they must pay. Proof of the type(s) of expense, the cost, and proof that it
was not paid by Medicare, Medicaid or a third party may be required. It is important that
new expenses or changes in current expenses are reported within ten days after receiving
a bill/receipt. Upload proof of medical expenses and other documentation to the My
ACCESS Account, or by fax at: 1-866-886-4342, or by mail to:
ACCESS Central Mail Center
P.O. Box 1770
Ocala, FL 34478-1770

SSI-Related Medicaid Fact Sheet 12
Special Policies that Apply to Spouses
Resources and income are evaluated for married individuals when one spouse is
institutionalized and receives Medicaid and one spouse continues to live in the community
(referred to as the “community spouse”) when applying for the ICP, Institutional Hospice,
HCBS Waiver (iBudget and SMMC LTC only) or PACE.
Resources at Application:
All resources of the couple must be counted together to determine the eligibility of the
institutionalized individual. After deducting $130,380 from their combined resources for the
community spouse resource allowance, the institutional spouse’s remaining resources must
not exceed $2,000 to qualify ($5,000 if the institutional spouse’s monthly income is $945 or
less).
Resources after Approval:
Resources over the individual limit ($2,000 or $5,000) acquired after Medicaid is
authorized must be transferred to the community spouse within twelve months after
approval to maintain eligibility.
Income at Application:
The total gross monthly income received by the institutionalized spouse applying for
Medicaid is considered in determining eligibility.
Allocation to the Community Spouse:
The allocation to the Community Spouse is referred to as the community spouse needs
allowance (CSNA). To calculate the amount that is allocated for the community spouse a
special budget is used to determine the personal needs allowance for the institutionalized
spouse, the income needs for the community spouse and patient responsibility.
Determining the Community Spouse Needs Allowance:
The following steps are used to determine the community spouse’s excess shelter costs:
Step 1 - Obtain verification of the community spouse’s monthly assistance group
expenses if questionable. Allowed expenses are limited to rent or mortgage payment
(including principal and interest), taxes, insurance (homeowners or renters), maintenance
charges if a condominium and mandatory homeowner’s association fees. Do not include
expenses paid by someone other than the community spouse. Add all of these
expenses.
Step 2 - To the total obtained above, add the current food stamp standard utility disregard
(refer to Appendix A-1) if the community spouse pays utility bills. Allowed utilities are
limited to water, sewage, gas, and electric.
Step 3 - To determine what portion of the total shelter costs is excess, subtract 30% of
the state’s income allowance, from the total costs. The difference is the community
spouse’s excess shelter costs.
SSI-Related Medicaid Fact Sheet 13
Exception:
If there is a court order for support that is greater than the above allowance, the court
ordered amount will be used as the community spouse allowance.
Other Dependents:
Under certain conditions, a dependent allowance may also be deducted from the
institutionalized individual’s income.
Note: The state's MMMNA plus CS excess shelter cost cannot exceed the state's cap on
CS income allowance (see Appendix A-9).
LONG-TERM CARE (LTC) INSURANCE PARTNERSHIP PROGRAM
What is the purpose of the Long-Term Care Insurance Partnership Program?
The Long-Term Care Insurance Partnership (LTCIP) Program is a federal and state
initiative intended to encourage individuals to plan for their future long-term care needs by
purchasing long-term care insurance policies.
How do I know if my policy is a qualified Long-Term Care Insurance Partnership
Program (LTCIP) policy?
The insurance policy must meet certain criteria and be certified by Florida’s Office of
Insurance Regulation (OIR) as a qualified LTCIP Program policy. Individuals purchasing or
owning a standard long-term care policy may contact and ask their insurance carrier about
purchasing or converting the current policy to a qualified LTCIP Program policy.
What is the benefit of a qualified Long-Term Care Insurance Partnership Program
policy?
The Department of Children and Families will not count a portion of an individual’s assets
if they apply for Medicaid to cover their nursing home care. The amount not counted is
equal to the actual amount of benefits paid out, or paid on their behalf, by the qualified
LTCIP Program policy for the individual’s cost of nursing home care.
For example, if the insurance company paid out $60,000 in benefits for John Doe’s care,
the State would not count $60,000 of his assets when Mr. Doe applies for Medicaid to
cover his ongoing care. In other words, Mr. Doe can keep $60,000 of his countable assets
above the ICP asset limit and still qualify for Medicaid if he meets all other eligibility
standards
What information do I need to provide to the Department when I apply?
Individuals with a qualified LTCIP Program Policy must provide documentation of the
insurance benefits paid out, or paid on their behalf, for the cost of their care. Contact
your insurance agency for assistance.
For more information regarding the Long-Term Care Insurance Partnership Program visit
:
http://ahca.myflorida.com/Medicaid/ltc_partnership_program/index.shtml,
http://training.floridashine.org/Website_Resources/Bene_FS/BLTCPartnership.pdf or
http://www.myfloridacfo.com/Division/Consumers/UnderstandingCoverage/LongTermCare
Overview.htm

SSI-Related Medicaid Fact Sheet 14
BUDGETING: CALCULATING PATIENT RESPONSIBILITY
Medicaid coverage for ICP, Hospice, HCBS (SMMC LTC and iBudget) and PACE may
have a patient responsibility based on the individual’s gross monthly income and where
the individual resides. The amount of the patient responsibility is determined by
subtracting the personal needs allowance (PNA) and other allowable deductions from the
individual’s gross monthly income. Please refer to DCF Policy Passage 2640.0118
Personal Needs Allowance for more details. The other allowances and deductions that
may apply are spousal and/or family allowance, court ordered child support only, and
uncovered medical expense deductions (UMEDS). The amount of the PNA is determined
by the coverage group and placement type at home, in a nursing facility, or an ALF.
For SMMC LTC and PACE, the PNA is as follows:
• Residing in a nursing facility is $130.
• Residing in an ALF is the ALF’s basic monthly Room and Board rate plus 20% of
the Federal Poverty Level (FPL).
• Residing in the community is 300% of the Federal Benefit Rate.
• For individuals residing in the community who are employed and receiving
HCBS/WPwD is 550% of the FBR.
Example 1:
The applicant applies and is approved for ICP and reports a nursing home expense
totaling $8,000 (UMED) prior to the month of approval.
Budget:
$1,300 monthly income - $130 Personal Needs Allowance (PNA) = $1,170
$1,170 x 6 months = $7,020
$8,000 nursing home bill - $7,020= $980 remaining balance of bill
$8,000/6 = $1,333.33 = $0 patient responsibility for each month
Since the nursing home bill exceeds the monthly income, use the remaining balance from
the bill when determining the patient responsibility for the next six months.
At the six-month review, the remaining balance of the nursing home bill of $980 is used
as an Uncovered Medical Expense Deduction (UMED).
Budget:
Remaining balance of bill $980/6 = $163.33
$1,040- $163.33 = $876.67 patient responsibility for each month
Example 2:
An individual is enrolled in the SMMC LTC program and resides in an ALF and has
Social Security Income of $1,750 each month. The ALF’s basic monthly Room and
Board rate is $1,500.
Budget:
$1,750 monthly income - $1,500 *ALF basic monthly rate - $202 (20% FPL) = $48 patient
responsibility for each month
*Note: This amount varies as it depends upon the facility’s actual room and board
SSI-Related Medicaid Fact Sheet 15
SSI-RELATED MEDICAID COVERAGE GROUPS WITH LIMITED BENEFITS
Medically Needy
•
Provides Medicaid to persons with medical bills, but whose income is too high to
qualify for full Medicaid coverage.
•
Individuals qualify for coverage on a month-to-month basis by meeting their
monthly share of cost.
•
More information may be found online at:
https://www.myflfamilies.com/service-programs/access/medicaid.shtml
Breast and Cervical Cancer Treatment (BCC)
•
For women needing treatment for breast and cervical cancer.
•
Must be screened and diagnosed for breast or cervical cancer by the
Department of Health (DOH).
•
Additional technical criteria include:
o
be uninsured or have health coverage that does not cover the necessary
treatment,
o
be under age 65,
o
be a U.S. citizen or qualified noncitizen, and
• Have income below 200% of the federal poverty level.
•
More information may be found online at:
http://www.doh.state.fl.us/Family/cancer/bcc/index.html
Qualified Medicare Beneficiaries (QMB)
•
Allows qualified individuals to have Medicaid pay for their Medicare premiums
(Part A and B), Medicare deductibles and Medicare coinsurance (within prescribed
limits). Individuals enrolled only in Medicare Part B, may be conditionally enrolled
in Medicare Part A after being determined eligible for the QMB Medicare Savings
Program (MSP).
•
An individual will automatically qualify for assistance with Medicare Prescription
Drug Plan costs through the Extra Help Program.
•
Additional technical criteria include entitlement to Medicare Part A.
•
Have income below 100% of the federal poverty level
.
Specified Low-Income Medicare Beneficiaries (SLMB)
•
Allows qualified individuals to have Medicaid pay for their Medicare Part B
premium.
•
an individual will automatically qualify for assistance with Medicare Prescription
Drug Plan costs through the Extra Help Program.
•
Additional technical criteria include enrolled in Medicare Part A.
•
Have income below 120% of the federal poverty level.
Qualifying Individuals 1 (QI-1)
•
Allows qualified individuals to have Medicaid pay for their Medicare Part B
premium.
•
Funding for this program is limited.
•
An individual will automatically qualify for assistance with Medicare
Prescription Drug Plan costs through the Extra Help Program.
•
Additional technical criteria include enrolled in Medicare Part A.

SSI-Related Medicaid Fact Sheet 16
•
Have income below 135% of the federal poverty level
.
NON-MEDICAID PROGRAMS
Optional State Supplementation (OSS)
•
Provides cash assistance to individuals residing in an assisted living facility (ALF),
mental health residential treatment facility (MHRTF), or adult family care home
(AFCH).
•
The supplemental payment is made directly to the individual and the amount is
based on the individual’s income and the current OSS standard cost of care in
the facility.
•
Some facilities are licensed to provide Assistive Care Services to individuals
who are Medicaid eligible.
•
Additional technical criteria include Certification by an Adult Services
Counselor, Developmental Disabilities Counselor, Mental Health Counselor or
the Aging and Disability Resource Centers (ADRCs) as needing placement in
a licensed facility (ALF, MHRTF, or AFCH).
Home Care for the Disabled Adult (HCDA)
•
Provides case management services and a small subsidy to approved caregivers
providing in-home care to adult persons with disabilities as an alternative to
institutional or nursing home care.
•
Payments are made directly to the provider/caregiver providing in-home care for the
disabled adult.
•
Eligibility is based on the financial status of the person receiving care.
•
Additional technical criteria include:
o
certification by a physician and an Adult Services case manager,
o
approval of the provider/caregiver, and
o
be between the ages of 18 and 59 and disabled.
Extra Help with Medicare Prescription Drug Plan Costs
•
Also known as the Low-Income Subsidy (LIS).
•
Medicare beneficiaries who qualify for QMB, SLMB and QI-1 are automatically
eligible for federal assistance with the costs of a Medicare prescription drug
plan.
•
All Medicare beneficiaries MUST enroll in a Medicare prescription drug plan to
obtain prescription drug coverage even if they qualify for the Extra Help Program.
•
Individuals are responsible for a small co-pay for each prescription.
•
LIS provides:
o
payment of all or most of the annual deductible,
o
coverage during the “doughnut hole” or gap period, and
o
payment of monthly plan premiums up to the base amount.
•
More information may be found online at:
https://www.medicare.gov/your-medicare-costs/get-help-paying-costs/find-your-level-of-
extra-help-part-d
SSI-Related Medicaid Fact Sheet 17
Additional Assistance Programs for Aged, Blind and Disabled
Public Assistance programs for aged, blind, and disabled individuals include food
assistance and Cash Assistance
.
Food Assistance:
•
The Food Assistance Program helps people with low-income buy healthy food. A
food assistance household is normally a group of people who live together and
buy food and cook meals together.
•
The SUNCAP Program is a special Food Assistance Program for individuals who
receive Supplemental Security Income (SSI). An individual may be eligible to
receive food assistance benefits through the SUNCAP Program without any
additional application, paperwork, or interview once they become SSI eligible.
Cash Assistance:
•
Supplemental Security Income (SSI) provides cash assistance and Medicaid to
eligible individuals and is administered by the Social Security Administration
(SSA). For more information, visit: https://www.ssa.gov/.
•
Optional State Supplementation (OSS) provides supplemental cash payments for
eligible individuals living in specially licensed living arrangements such as Assisted
Living Facilities and is administered by the Department of Children and Families.
•
Home Care for the Disabled Adult (HCDA) provides case management services
and a small financial subsidy to approved caregivers providing in-home care to
disabled adults (ages 18 through 59) as an alternative to institutional or nursing
home placement and is also administered by the Department of Children and
Families.
ADDITIONAL RESOURCES
SSI recipients may contact 850-300-4DCF (4323) to request a lost or stolen Medicaid
card. Individuals with a MyACCESS Account can request a replacement Medicaid card
at: http://www.myflorida.com/accessflorida/
Social Security Administration (SSA)
For more information about or to apply for benefits available through the Social Security
Administration (retirement, disability insurance, Supplemental Security Income, Extra Help
with Medicare Prescription Drug Plan costs), call the Social Security Administration at 1-
800-772-1213, visit a local SSA Office or visit the SSA website at: http://www.ssa.gov/.
Medicare
Medicare is a federal health insurance program that includes hospital insurance (Part A),
medical insurance (Part B), Medicare HMO plans (Medicare Advantage), and Medicare
prescription drug plans (Part D). For information about Medicare coverage, call 1-800-
633
-4227
or visit the Medicare website on- line at: http://www.medicare.gov.
SSI-Related Medicaid Fact Sheet 18
Florida Discount Drug Card
Individuals who are not eligible for full Medicaid may receive help with the cost of
prescription drugs through the Florida Discount Drug Card at:
http://www.floridadiscountdrugcard.com/
.
Florida Elder Helpline and Referral
Information regarding elder services and activities is available through the Elder Helpline
Information and Referral Service within each Florida County at: 1-800-96-ELDER (1-800-
963-5337).
All elder help lines may be accessed through the Florida Telecommunication Relay
System (1-800-955- 8771 for TDD, or 1-800-955-8770 for Voice), which allows telephone
calls to be placed between TDD users and nonusers with the help of specially trained
operators translating the calls.
Information is also available on the internet at: Elder Affairs Helpline
A listing by Area Agency on Aging is also available.
My ACCESS Account – Provider View Guide
Provider View provides you with a secure gateway to the customers “account” information.
The Provider View system allows you to view customer case information and interact with
the Department of Children and Families through the Web at your convenience twenty-
four hours a day seven days a week
Provider View (Check Information about Medicaid eligibility) allows you to:
• View current benefits for Medicaid
• View the date benefits will be available
• See when the next review is due
• See when an appointment is scheduled
• View Medicaid account history
• View Medicaid Patient Responsibility
• View a list of verifications needed
• View Personal Identification number (PIN)
• View a list of Applications that have been submitted
• View a list of Changes that have been submitted
• View a list of Requests for Additional Assistance
• View a list of Reviews that have been submitted
The information displayed in the customer’s account is updated nightly. Changes made
during the day are available for you to view the following day. The date of the information
is displayed at the top of the account status screens for reference.
Click here to go to the My ACCESS Account – Provider View Guide.
SSI-Related Medicaid Fact Sheet 19
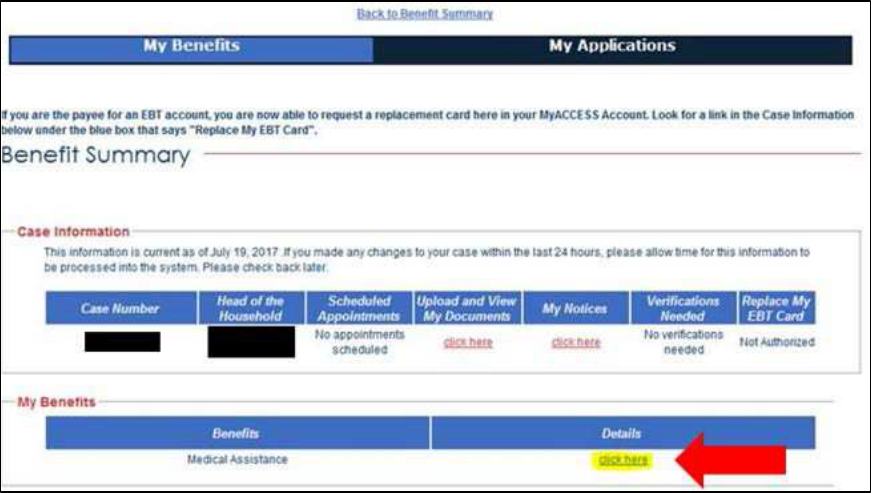
Where to Find Customer’s Patient Responsibility Amount in Provider View
Log into ‘Provider View’ and complete ‘Customer Search’ to find the individual you want to
review.
• To begin start at is the “My Benefits” screen – Refer to page 8 of Provider View
Guide.
• Select ‘Click Here’ under Details section for Medical Assistance (see Figure 1.1
below).
Figure 1.1 Benefit Summary Page in Provider View
This will take you to the Medical Assistance page.
SSI-Related Medicaid Fact Sheet 20
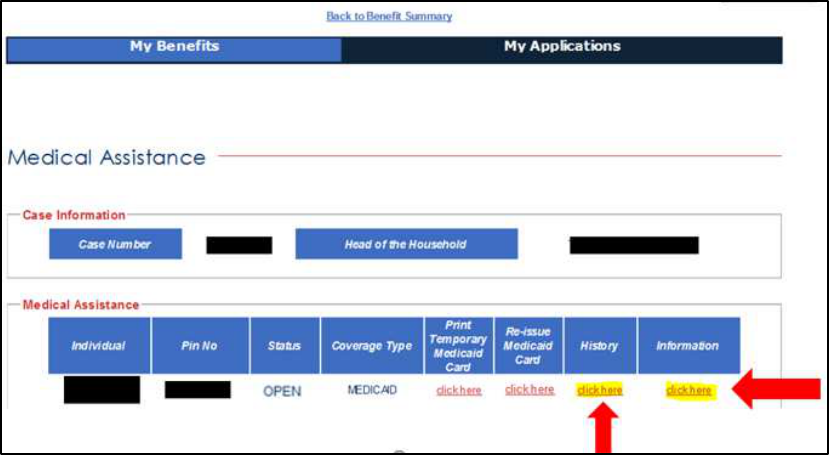
Medical Assistance Page
On this page you can view current month’s patient responsibility amount by selecting ‘click
here’ under ‘Information’ section or to view previous month’s patient responsibility amount
under ‘History’ section (see Figure 1.2 below). Note: The “Re-issue Medicaid Card” field is
not available to Providers.
Figure 1.2 Medical Assistance Page in Provider View
